
According to the World Health Organization (WHO), 1 in 100 children suffers from a neuro-developmental disorder known as autism spectrum disorder (ASD). Although the term may seem complicated, it refers to a broad range of conditions marked by difficulties with speech, nonverbal communication, social skills, and repetitive behaviors. It is well known that there are a wide range of strengths and difficulties among people with ASD. People with Autism Spectrum Disorder (ASD) can learn, reason, and solve problems in a variety of ways, from very proficient to very challenged. It presents a special challenge in the field of medical diagnostics because of its spectrum and the range of degrees of manifestation.
Traditionally, diagnosing ASD involves a two-stage process.
- General developmental screening: Doctors, particularly pediatricians, frequently perform developmental surveillance during well-child exams. If developmental delay symptoms are identified, a more thorough test tailored to ASD is conducted.
- Comprehensive ASD evaluation: This calls for a comprehensive evaluation by specialists, such as developmental pediatricians, neurologists, and psychologists. They will assess the age-appropriate skills, linguistic proficiency, and cognitive level or thinking abilities needed to carry out daily tasks, including eating, dressing, and using the restroom on their own.
It sounds thorough, doesn’t it? Nonetheless, these procedures have significant shortcomings:
- Time-consuming: It takes a while to receive an ASD diagnosis because many evaluations by different specialists are required. Families may have to wait a long time to see a doctor, much less receive a definitive diagnosis.
- Subjectivity: Diverse judgments could result from the adoption of slightly different standards or criteria by each specialist in their examinations.
- Access and equity: Not every child has simple access to a comprehensive evaluation—particularly in settings with limited resources or in underprivileged areas. Furthermore, biases may enter the picture unintentionally or knowingly, impacting the diagnostic process.
- Costly: The diagnostic process can be emotionally and financially draining due to the possibility of increasing medical expenses from multiple evaluations, frequently conducted over extended periods.
These flaws aren’t simply inconvenient; they can cause serious delays in a child’s developmental path, especially in light of the critical need for early identification and intervention in ASD. Therefore, it is not only necessary but also important to look for a more effective, objective, and approachable answer.
The emergence of Artificial Intelligence (AI)
The complex field of autism spectrum disorder (ASD) diagnosis can be difficult and time-consuming to navigate; it can be like trying to find a needle in a haystack. Healthcare and artificial intelligence (AI) together have the potential to completely transform this process, making it quick and accurate. Now, let’s explore more:
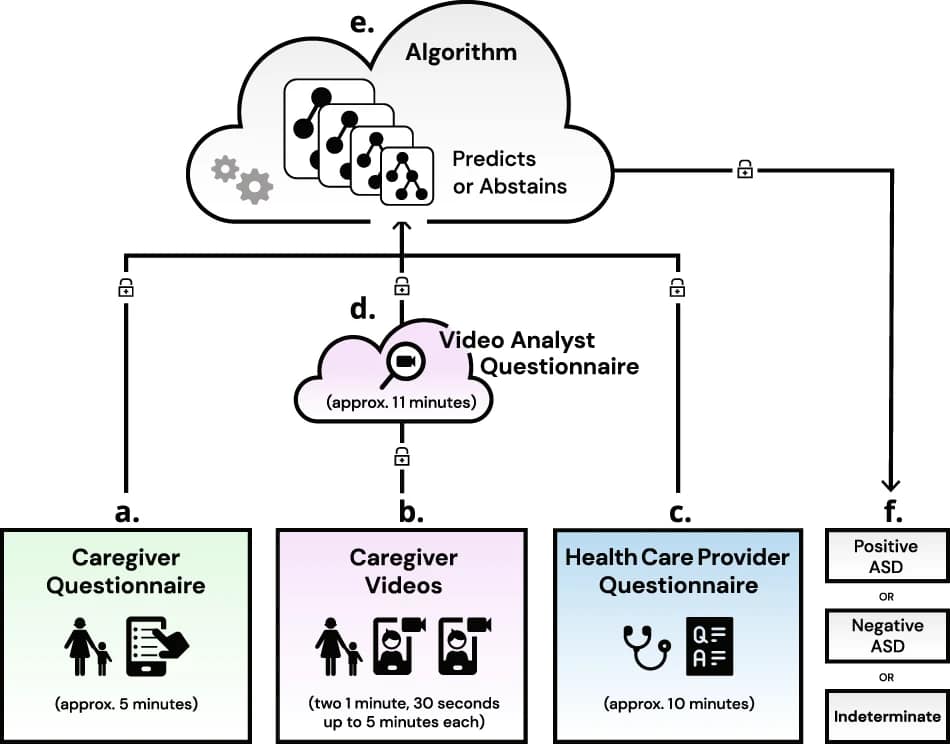
- Software as a Medical Device (SaMD):
- This is a software program, not hardware, used for medical purposes. Software meant for the diagnosis or recommendation of disorders such as ASD is referred to here as SaMD.
It leverages the following data types:
- Caregiver questionnaires: Caregivers provide valuable information through questionnaires, which include details about the child’s behavior, development, and interactions. These questionnaires offer insights into the child’s social, communication, and behavioral patterns.
- Video analysis: Caregivers capture and submit videos of the child in natural settings, such as during play or interaction. These videos are used for observational analysis, allowing experts to assess the child’s behavior, social interactions, and communication skills.
- Healthcare Provider (HCP) questionnaires: Healthcare providers complete questionnaires based on their assessment during in-person or remote visits with the child and caregiver. These questionnaires add a professional evaluation to the diagnostic process.
- Demographic data: Demographic information about the child, caregiver, and family is collected, including age, sex, race/ethnicity, parental education, and income. This data helps evaluate performance variability among subgroups and accounts for disparities in ASD diagnosis.
- Machine Learning (ML):
- ML, a branch of AI, enables computers to learn from data and make judgments without explicit programming. For example, ML can identify patterns or markers suggestive of ASD by examining large volumes of patient data.
The AI-driven solution for ASD:
- Diagnostic solution:
- Yes, the main purpose of the solution is diagnostic. But it offers objective, data-driven insights rather than depending just on subjective assessments, revolutionizing the way ASD is recognized.
- It is essentially a SaMD. It uses a strong software solution that makes use of a machine-learning algorithm, not a physical device. The enormous volumes of data the algorithm processes allow it to learn and improve its diagnostic abilities.
The SaMD in action:
The real testament to the power of this technology isn’t just in its design but also in its performance.
- Participants and data scope:
- Initially, 711 people were enlisted, and over 425 of them went through with the study average age of 3.33 years, and those with ASD averaged 2.96 years. Such a vast amount of data provides fertile ground for ML to operate, refining its detection capabilities.
- Healthcare providers’ involvement:
- The software was used by 15 healthcare professionals, both male and female, with an average experience level of 16 years, and they confirmed its usability and practicality.
- Definitive results:
- Out of all participants, the software gave a definitive ASD diagnosis for almost 32% of them, translating to objective, quick, and precise results.
- Performance metrics:
- Positive Predictive Value (PPV) and Negative Predictive Value (NPV):
- In simple terms, PPV and NPV indicate the probability of the software correctly identifying ASD and non-ASD cases, respectively. The software achieved a PPV of 80.8% and an NPV of 98.3%.
- Sensitivity and specificity:
- Sensitivity is the ability to correctly identify those with ASD, and specificity is the ability to exclude those without. The SaMD showed a sensitivity of 98.4% and a specificity of 78.9%.
- Positive Predictive Value (PPV) and Negative Predictive Value (NPV):
The SaMD has enormous potential for primary care settings because it was created to expedite the diagnosis of autism spectrum disorder (ASD). But to effectively support global health parity, this AI-driven solution must blend in with a variety of settings, particularly those with few resources. Here, we go into greater detail on the difficulties and customized fixes that are necessary for the SaMD’s effective implementation in real-world settings.
Navigating implementation challenges:
- Scalability in diverse demographics:
- Challenge: The SaMD was first tested on a sample of 425 participants, and it is important to recognize how difficult it will be to scale up to larger groups. A more extensive and heterogeneous cohort could exhibit complex ASD symptoms or co-occurring neuro-developmental disorders, which could impact the specific rates of the SaMD.
- Solution: Provide data from different parts of the world to the AI algorithm iteratively. To document all possible ASD manifestations, work with regional health organizations.
- Cultural and linguistic nuances:
- Challenge: Different cultural groups may have different interpretations of the caregiver questionnaire, which is an essential component of the SaMD. This can be made worse by linguistic hurdles, which could distort the outcomes.
- Solution: To improve the questionnaire, closely collaborate with linguists and cultural anthropologists in particular areas. Ensure clarity and accuracy in data gathering by implementing a multilingual interface and context-specific prompts.
- Infrastructure limitations:
- Challenge: Real-time data processing may be hampered by unreliable internet connectivity or restricted access to SaMD-compatible devices in low-resource environments.
- Solution: Make the SaMD compatible with more devices, even those from earlier generations of technology. Create an offline version that enables data entry and basic processing; it can then sync and update when connectivity is restored.
- Skill gaps among healthcare providers:
- Challenge: The study’s fifteen HCPs averaged sixteen years of post-residency experience. On the other hand, medical professionals in many low-resource environments might not have much background in ASD, much less a cutting-edge AI diagnostic tool.
- Solution: Launch training programs tailored to the needs of the region, using regional medical educators. To accelerate the learning curve, incorporate real-world examples into case-based learning.
The creation of the SaMD signifies a major advancement in the revolution of ASD diagnosis. The path from study to widespread implementation is fraught with difficulties, but it is necessary to guarantee that every kid, regardless of circumstances, receives a prompt and correct diagnosis. The SaMD has the potential to be a powerful tool for change, bringing in a new era of global health equity, by precisely and proactively addressing these issues.
Imagine living in a society where access to technological improvements in healthcare is commonplace rather than a privilege. In what ways can we work together, be creative, and make investments to make this vision a reality?
Source article: https://www.nature.com/articles/s41746-022-00598-6#Fig1
Disclaimer: Please note that the opinions, content, and analysis in my posts are entirely my own and do not reflect the views of any current or past employers or institutional affiliations. These posts, based solely on publicly available information, are for informational purposes and should not be taken as professional advice. All insights and conclusions are my viewpoints and should not be considered representative of any organizations I am or have been associated with. This content is not endorsed by, nor does it represent the stance of any affiliated entity.





