
The future of healthcare lies in making better, more informed decisions rather than relying solely on complex surgeries or new medications. A crucial area that has been overlooked is the prediction of neurological outcomes following resuscitation. However, AI may be about to provide a game-changing solution.
Predicting neurological outcomes is a formidable challenge at the core of post-resuscitation care. Once a patient has undergone cardiopulmonary arrest outside of a hospital, it’s important to assess how their brain has responded and what their chances of recovery are. In the past, physical examinations and preliminary CT (Computed Tomography) scans have been our tools for this.
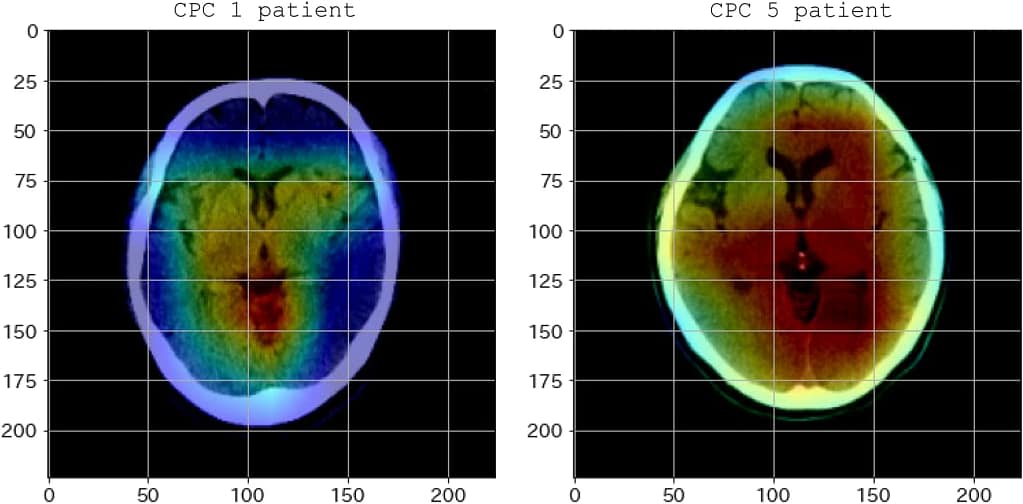
Advanced imaging techniques, such as CT scans, offer a detailed picture of the internal organs and tissues of the body. Within the post-resuscitation setting, they provide insight into the brain’s condition. However, even though they are valuable, their readings are frequently unclear, particularly in the first few hours following resuscitation. It is a fundamental limitation of the technology rather than a technical error that causes a lack of clarity. The binary nature of CT scans makes it difficult to distinguish between recoverable brain function and irreversible damage. This is where the current tools falter.
The clinical implication:
- Prediction ambiguity is more than just a minor inconvenience. It results in important clinical conundrums. In the absence of clear insights, doctors may be unduly optimistic or prematurely pessimistic. Both may cause the care pathway to become skewed; the former may result in lengthy treatments that are not very beneficial, while the latter may cause opportunities for recovery to be missed. Ambiguity affects life-altering decisions in the medical field and is not just a professional but also a deeply personal challenge.
AI-driven solution
Artificial intelligence (AI) has proven to be a powerful ally in the healthcare industry, as it has made considerable advancements over the years. AI has frequently demonstrated its potential, from forecasting patient influx in emergency rooms to helping with radiology interpretations. However, AI is like a digital surgeon when it comes to interpreting neurological outcomes after resuscitation; it’s more than just an ally in this regard. The human touch is not replaced; rather, data-driven insights are used to enhance it.
The VGG19 model is a deep learning model, which means that it is built to learn and think similarly to a human brain but with the ability to process large amounts of data quickly. VGG19, which was initially created for image recognition, is capable of carefully examining images to find patterns and features that the human eye might miss or interpret as unclear.
- Nature of the tool:
- The VGG19 model is a predictive tool. Analyzing post-resuscitation CT scans and forecasting neurological outcomes is its main duty. The AI-driven VGG19 model offers a data-backed prediction based on deep patterns within these images, in contrast to conventional CT scans that deliver raw images open to interpretation.
- What makes AI a superior contender?
- The AI-driven model’s superiority over traditional methods is multifaceted.
- Depth of analysis: Traditional tools provide a surface-level view, while the VGG19 delves deep, analyzing intricate patterns.
- Speed: While a human may take hours to pore over CT scans, VGG19 offers rapid predictions.
- Objectivity: Human analysis can sometimes be swayed by bias or fatigue. In contrast, the VGG19 model maintains consistent objectivity.
- Adaptive learning: The more data the VGG19 model processes, the better its predictions become, thanks to its learning capabilities. This means its efficacy isn’t static; it’s ever-improving.
- The AI-driven model’s superiority over traditional methods is multifaceted.
- Fresh insights from AI:
- A significant improvement is the subtle differentiation made between irreversible and recoverable brain damage. Traditional approaches frequently produce binary results—good or bad—because of their inherent limitations. However, ranges or spectra of results can be indicated by the VGG19 model. A highly customized treatment plan versus one that is more broadly applicable may depend on this specific information.
However, the theoretical strength of any instrument is as good as how well it performs in practice. The VGG19 model looks promising in this regard. The research yielded a Receiver Operating Characteristic – Area Under the Curve (ROC-AUC) of 0.84. Stated differently, this indicates the degree to which the model can discriminate between favorable and unfavorable results; a score of 0.84 is noticeably high. Additionally, the model’s accuracy was demonstrated even in datasets with imbalances, as evidenced by its PR-AUC (Precision Recall – AUC) of 0.73.
The VGG19 model exhibits superior performance or comparable results when compared to conventional methods that utilize the conventional Gray-to-White matter ratio (GWR) from the same images. This suggests that the VGG19 model has great potential as a leading tool for neurological outcome prediction.
Possible challenges that might hinder the scalability of the innovation and accompanying solutions
Uncovering AI’s potential in healthcare presents some complex challenges, particularly in terms of forecasting neurological outcomes after resuscitation. We struggle not only to apply this research to the day-to-day activities of clinical practice but also to modify it for a variety of global, low-resource contexts.
Challenge: Ethical concerns surrounding AI predictions in critical care
- An artificial intelligence model’s prediction has significant ramifications for post-resuscitation care. The choice to pursue aggressive treatment or think about receiving end-of-life care is a deeply personal and complex one. Heavily depending on the prediction of an AI model may inadvertently oversimplify this decision-making process, possibly sidelining the holistic understanding of the patient’s health and contextual circumstances.
Solution: Human-AI Collaboration Framework
- The solution is to build a synergy between AI and human intuition rather than to pick one over the other. The preservation of human judgment is ensured by a structured framework in which AI offers a strong recommendation but leaves the final call to an experienced clinician. In this case, artificial intelligence serves as an augmented intelligence tool, enhancing rather than substituting the clinician’s insights.
- Furthermore, interpretability tools that deconstruct AI predictions should be made available to clinicians. They can make better decisions if they know why the AI model made a specific prediction, regardless of whether it was based on patterns in the basal ganglia or other parts of the brain.
Challenge: Technical infrastructure shortcomings
- It’s possible that environments with limited resources lack the sophisticated hardware required to run cutting-edge AI models. Furthermore, there might not be as much reliable and high-quality data available to train these models.
Solution: Cloud-based AI and collaborative data collection
- Through the use of cloud-based AI solutions, healthcare facilities can do away with expensive local computational infrastructure. With this method, processing-intensive tasks can be carried out on remote servers that are reachable from almost anywhere.
- Additionally, a cooperative labeling project involving various hospitals and clinics can generate a pooled dataset, improving the quality of the AI’s training data and increasing its effectiveness.
Moving forward means navigating a complex terrain of ethics, resources, and cultural dynamics in addition to taking on a technological challenge. There are several ways to address the issue, and as we work toward achieving global health equity, the way forward becomes more obvious.
One question still needs to be answered as we continue on this journey: How can we make sure that, despite AI’s transformation of healthcare, the values of inclusivity, compassion, and trust are at its core?
Source Article: https://www.nature.com/articles/s41598-023-32899-5#Fig3
Disclaimer: Please note that the opinions, content, and analysis in my posts are entirely my own and do not reflect the views of any current or past employers or institutional affiliations. These posts, based solely on publicly available information, are for informational purposes and should not be taken as professional advice. All insights and conclusions are my viewpoints and should not be considered representative of any organizations I am or have been associated with. This content is not endorsed by, nor does it represent the stance of any affiliated entity.





