
End-stage lung illness is a complex issue that often results in the urgent need for a lung transplant. Both patients and medical professionals are constantly threatened by the availability, or rather, the glaring scarcity, of viable donor lungs. Despite their clinical validation, conventional techniques of evaluation still face uncertainty when evaluating possible donor lungs. Particularly in a field where every single organ matters, these customary techniques may occasionally toss out organs that, while questionable, may be viable for transplant. To avoid any potential life-saving opportunity being missed owing to methodological restrictions, the urgent issue is not just organ shortage but also the suboptimal handling of available organs.
Impact of donor lung scarcity
The persistent donor lung scarcity has a wide-ranging impact that extends beyond the immediate care team to patients, their families, and the healthcare system at large. Some of these include:
- Patient suffering: There is a significant and measurable human cost. Breathlessness, a lower quality of life, and the looming feeling that time is running out are common experiences for patients with end-stage lung illness. Their physical pain and emotional anguish are made worse by the lengthy lung transplant waiting times.
- Ethical dilemmas: It could be potentially unethical to discard possibly healthy lungs because of the shortcomings of conventional diagnostic techniques. The consequent organ wastage highlights a significant gap that has to be addressed when compared to the urgent need for such organs.
- Healthcare strain: The larger healthcare system is also affected, in addition to the direct stakeholders. Rare organ supply results in extended intensive care unit stay for patients, higher expenses for ongoing medical treatment, and increased resource allocation, all of which put further strain on the already strained healthcare system.
- Morbidity and mortality issues: The risk increases as each second goes by. The lack of healthy donor lungs always results in higher transplant-related mortality rates and higher levels of morbidity among those who experience a negative decrease in their health while waiting.
- Family and social impact: Families and caregivers are affected more greatly, and there, the financial, emotional, and physical strain becomes a constant worry. It is impossible to overstate the level of ongoing stress and anxiety felt by families as they simultaneously wait in anticipation and fear for a transplant that could save their loved one’s life.
AI-powered solution and measurable impact
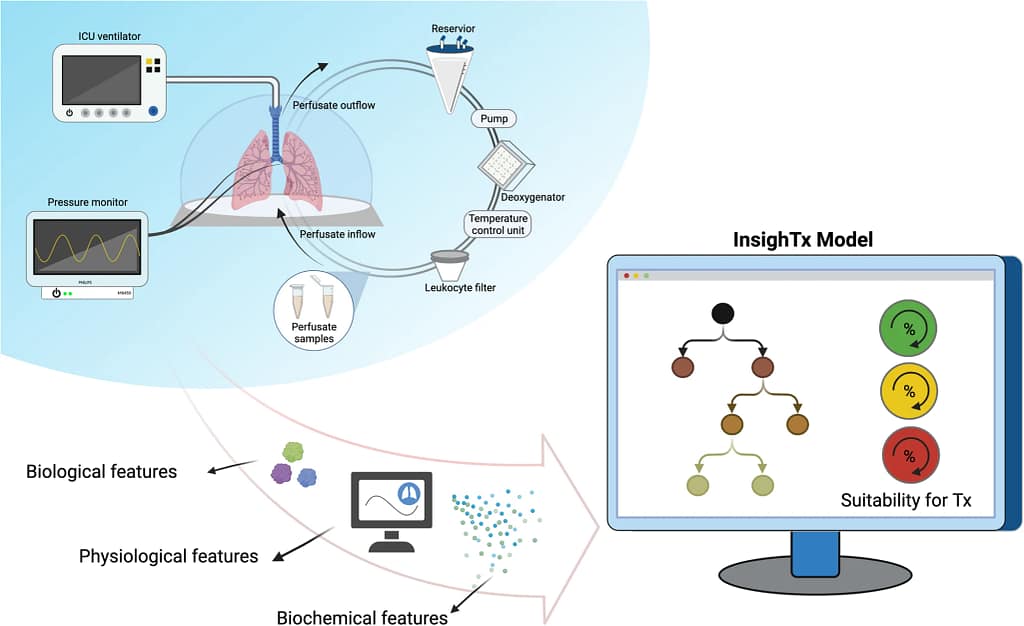
A tool like the InsighTx model, a breakthrough created to improve the predictability of post-transplant outcomes, was necessary for navigating the complex world of organ transplantation. At its core, this model integrates technology and medical knowledge to enable a more educated, data-driven approach to evaluating the suitability of lungs for transplantation, filling the important gaps left by conventional assessment techniques.
Exploring the InsighTx model’s technological foundation reveals a careful application of machine learning, a type of artificial intelligence that allows systems to learn from data. Through EVLP (Ex Vivo Lung Perfusion), which evaluates and enhances the functionality of donor lungs outside the body before transplantation, a more nuanced and predictive analysis is provided. The model, which was trained and validated using a substantial dataset of 725 EVLP cases, sifts through a plethora of factors and provides a level of scrutiny and precision that is not possible with traditional evaluation techniques.
The model’s effectiveness is measured using measures known as AUROC (Area Under the Receiver Operating Characteristic Curve), or a measure of a model’s ability to distinguish between classes, in this case, viable and non-viable lungs for transplant. These measures enable better decision-making in lung transplants by validating the model’s dependability and solidity and by offering a formal, numerical basis to assess its predictive power.
The use of the InsighTx model went beyond its theoretical usefulness and had a significant impact on transplantation outcomes. The model demonstrated its reliability as a tool by displaying an AUROC of 79+3% during its training phase and was verified by test datasets that showed an AUROC between 75+4% and 85+3%. It also highlighted its practical relevance in real-world circumstances.
With an AUROC of 90+4% and an AUROC of 80+4%, respectively, it stands out in particular for its ability to accurately identify unsuitable lungs for transplantation and predict favorable transplant outcomes. In a practical setting, the model significantly reduced the risk of transplanting less-than-ideal lungs and increased the likelihood of choosing appropriate ones. Odds ratios, a statistical measure used to identify the strength and direction of an association between two conditions, paint a compelling picture of its practical effectiveness
Thus, the introduction and integration of the InsighTx model represent a fusion of medical and technological expertise, providing a glimpse into a future in which technological interventions like machine learning pave the way for improved global health outcomes, particularly in the complex and crucial field of organ transplantation.
Challenges that might hinder scalability and possible solutions
In the field of organ transplantation in particular, it is crucial to ensure that solutions like the InsighTx model seamlessly translate from research to practical use. It is critical to carefully combine theory, real-world application, and scalability, especially while managing the inherent limitations and difficulties in various healthcare systems. Some of the challenges that can be encountered and accompanying solutions include:
A. Data collation
Problem: Data quality and volume differences between regions may be encountered during the model’s validation using 725 EVLP examples.
Solution:
- Create and execute standardized data management and gathering procedures for use by healthcare organizations.
- Create collaborative platforms for institutional knowledge and data sharing to synchronize practices around the world.
B. Technological expertise & infrastructure
Problem: A machine-learning model like InsighTx could be difficult to develop and keep up-to-date in low-resource environments due to a lack of resources and specialized skills.
Solution:
- Establish projects to exchange information and resources in order to close knowledge and skill gaps.
- Create initiatives for the transfer of technologies and partnerships between academic institutions and healthcare organizations in low-resource environments.
C. Ethical and regulatory requirements
Problem: It is a complex requirement to ensure compliance with various legal and ethical rules in various parts of the world.
Solution:
- Engage in cooperative discussions with regulatory organizations worldwide to guarantee ethical and legal observance.
- Encourage the creation of international regulations or rules that are specialized for using AI models in healthcare.
Integrating these solutions is crucial, both as a way to address local and regional problems and as a planned effort to democratize healthcare technology. A richer, more evenly distributed technological impact in healthcare is fostered by the combination of collaborative, scalable, and inclusive solutions, particularly with the InsighTx paradigm.
The potential to implement innovations like the InsighTx model across many socioeconomic terrains is tangible if tactics and structures go beyond locally focused solutions and integrate themselves within a global framework. Such a trajectory not only ensures that healthcare innovations are not constrained in high-resource settings but also validates their impact and applicability across a wide range of healthcare environments, closing the equity gaps in global health.
We recognize and value the advances achieved by the InsighTx model in boosting prediction abilities in the transplantation sector. It has obvious and critical potential to enhance lung usability and patient outcomes. The path to achieving global health equity in transplantation science is still being paved, nevertheless.
How can we, as a group of healthcare professionals, technologists, and global citizens, further coordinate our actions to ensure that advancements in transplantation science are not only technologically revolutionary but also fairly accessible and applicable globally? This is a question that is best answered with the insights and technological prowess provided by models like InsighTx.
Source article: https://www.nature.com/articles/s41467-023-40468-7
Disclaimer: Please note that the opinions, content, and analysis in my posts are entirely my own and do not reflect the views of any current or past employers or institutional affiliations. These posts, based solely on publicly available information, are for informational purposes and should not be taken as professional advice. All insights and conclusions are my viewpoints and should not be considered representative of any organizations I am or have been associated with. This content is not endorsed by, nor does it represent the stance of any affiliated entity.





